At the 2023 ECNP Congress in Barcelona, Spain (7−10th Oct), two symposia explored the importance of considering patient life engagement as a treatment goal for individuals with schizophrenia. The first was titled, ‘Therapeutic outcomes in schizophrenia: the importance of patient life engagement’. In this session, Dr John M Kane (Hofstra/Northwell University, USA) spoke first to provide a detailed explanation about what patient life engagement is and why it is relevant to the ongoing treatment of schizophrenia.1 Dr Martha Sajatovic (University Hospitals Cleveland Medical Center, USA) then followed to explain how we can assess patient life engagement with our patients and what this means for treatment choice.2 The second industry session was titled ‘Improving functional outcomes and life engagement: new goals for individuals living with schizophrenia’, in which Dr Greg Mattingly (Washington University, USA) explained that our choice of treatment has a key role to play when considering patient life engagement.3
What is patient life engagement and how is it relevant in schizophrenia?
There is a need to incorporate the patient’s perspective in treatment planning and goal setting in schizophrenia
In the past, said Dr Kane, physicians treating schizophrenia have mainly aimed for symptom control, with adverse reactions of treatment viewed as a small price to pay.1 Yet for patients with schizophrenia this focus has frequently led to poor medication adherence, incomplete functional recovery, poor quality of life, and ultimately symptom relapse.1,4-6 Evidence shows that adverse events from antipsychotics impact social functioning in 82% to 91% of patients with schizophrenia.7 There is therefore a growing need to incorporate the patient’s perspective in treatment planning and goal setting in order to help address these issues, which is where the concept of patient life engagement comes in.8
Patient life engagement refers to the positive health aspects relating to cognition, vitality, motivation and reward, and the ability to feel pleasure.9 Examples provided by the speaker included having a relationship or family, finding employment, going back to school, or improving physical condition.1,8 Studies indicate that incorporating the patient’s perspective can have positive outcomes on treatment adherence,10 satisfaction and confidence,10 while fostering a therapeutic alliance with their clinician.8
Incorporating the patient’s perspective can have positive outcomes on treatment adherence, satisfaction and confidence
Assessing patient life engagement and current treatment options
Dr Sajatovic reaffirmed the need to think beyond symptom control, explaining that treatment priorities in schizophrenia frequently differ between the patient and the clinician.11 In a 2013 study, patients with schizophrenia were found to place more priority on activities of daily living and work, while their physicians prioritized improving symptoms and cognition.11 Such discordance between the two priorities may lead to treatment non-adherence.2
Guidelines for treating schizophrenia encourage the inclusion of patient preferences in treatment planning.12-14 Patient-centered discussions, Dr Sajatovic said, could achieve this by providing insight into patients’ treatment goals and personal barriers. This can include asking “What are your goals for recovery?” and “What are barriers to regular medication-taking for you?”2
There is currently no specific measure of patient life engagement for patients with schizophrenia
Dr Sajatovic did admit though that there is currently no specific measure of patient life engagement for patients with schizophrenia.15 Many available outcome measures do cover aspects of patient life engagement, including patient well-being, quality of life, treatment satisfaction and the therapeutic relationship, but none specifically measure it.15 An appropriate outcome measure would allow physicians to attain an holistic understanding of a patient’s feelings, activities, satisfaction and priorities and in the symposium, Dr Sajatovic discussed some items from the Positive and Negative Syndrome Scale that were seen as relevant in the assessment of life engagement.8
Before providing some example case studies, Dr Sajatovic laid out three key points for optimizing patient life engagement and functioning in patients with schizophrenia from her own clinical experience:2
- Clinicians and patients should collaborate (shared decision-making) on treatment goals
- Collaborative decision-making can help to clarify benefit versus burden of medication and inform treatment planning
- Optimizing life engagement is a continuous process, and medication needs to be regularly re-assessed for appropriateness
Improving functional outcomes and life engagement: new goals for individuals living with schizophrenia
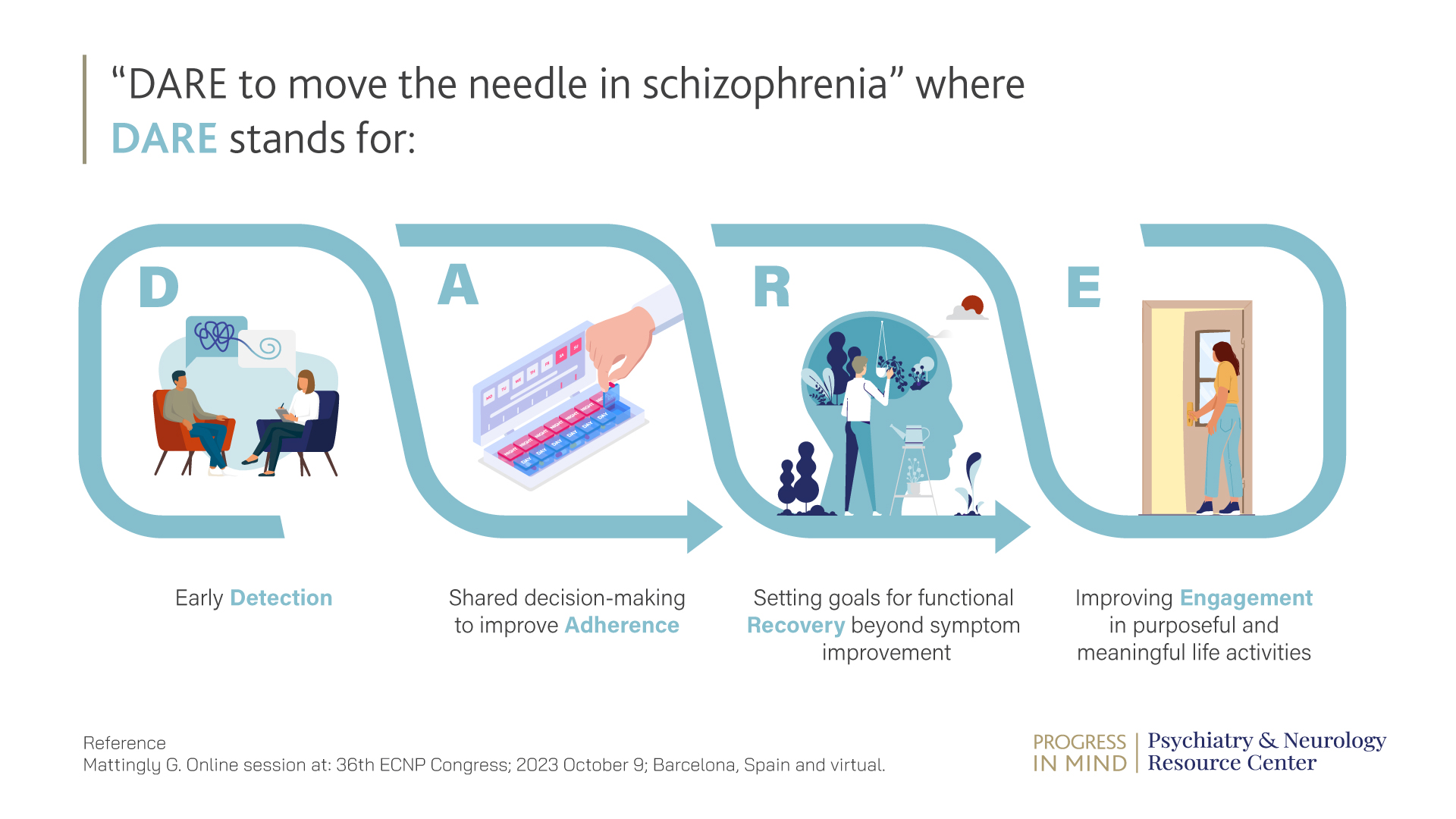
The need to assess the appropriateness of medication to optimize life engagement in patients with schizophrenia was a key message from Dr Mattingly’s presentation.3 This session began with the speaker asking the audience to “DARE to move the needle in schizophrenia”. The acronym DARE stands for early Detection, shared decision making to improve Adherence, setting goals for functional Recovery beyond symptom improvement, and improving Engagement in purposeful and meaningful life activities.3
Patients, Dr Mattingly said, focus on the tolerability of their medication. In one survey of 1,825 patients with psychosis from 2010, 61% of patients reported impairment in their daily life as a result of adverse events from medication, such as being tired or gaining weight.3,16 Not addressing this issue is leading to long term distress, Dr Mattingly added.3 There is therefore a need for treatments that can improve the symptoms of schizophrenia, as well as cognition and quality of life, but with limited adverse events such as weight gain.3
There is a need to assess the appropriateness of the medication to optimize life engagement in patients with schizophrenia
An appropriate summary came from Dr Sajatovic, who said that in the vast majority of cases, considering patient life engagement should now be a fundamental part of care in schizophrenia and, with the appropriate structures and resources in place, patients with schizophrenia will have increased ability to engage with the world and regain functioning, and engagement with life.2
Educational financial support for the first Satellite symposium was provided by Otsuka Pharmaceutical Europe Ltd. and H. Lundbeck A/S, and for the second Satellite symposium by Angelini Pharma.
ECNP: European Collegge of Neuropsychopharmacology
USA: United States of America
DARE: early Detection, shared decision making to improve Adherence, setting goals for functional Recovery beyond symptom improvement, and improvising Engagement in purposeful and meaningful activities.
BE-NOTPR-0365, approved:01/2024